Staff Perspective: I Did Not Sign Up for this Ultra-Marathon: Challenges to Providing Evidence-Based Psychotherapy in 2023
Practicing as a mental health clinician over the past few years has felt like running in an ultra-marathon. Not that I would ever voluntarily participate in such an endeavor. But I similarly did not voluntarily choose to confront the myriad of hurdles to clinical work since 2020: a global pandemic and its associated challenges, political and economic upheaval, heightened awareness of systemic racial violence, and continuing threats of war.
As a clinician, you’re likely well aware that the need and demand for mental health treatment has increased dramatically as a result. My practice has been full for over a year. Despite having discontinued all of my marketing, I still receive frequent inquiries, both from potential clients and other providers, because it is so difficult to locate mental health providers whose caseloads aren’t also full. Unfortunately, this isn’t unique to my geographical or specialty area. While the demand for services has increased, so has the number of mental health providers exiting the field. The American Psychological Association (APA, 2022) reported on the results of their national 2022 COVID-19 Practitioner Impact Survey. Some of the relevant lowlights include:
- 46% of psychologists reported being unable to meet the demand for treatment.
- 67% of psychologists reported having no openings for new patients.
- 38% of psychologists maintained a waitlist for their practice.
- 43% of psychologists reported seeing more patients than they did prior to the COVID-19 pandemic.
Although the APA survey focused on psychologists, it’s reasonable to assume that similar trends exist for other mental health care providers.
While our clinical practices are booming, the personal toll is significant. The APA survey noted that 45% of psychologists endorsed feeling burned out. The reality is that providers are trying their best to meet their clients’ needs while facing the same myriad of public health stressors. I know many effective CBT interventions, but that doesn’t always combat my anxiety when a family member gets diagnosed with COVID-19 or my retirement account plummets.It’s hard to keep my own mood in check when the news reports the death toll from the latest mass shooting or the most recent victim of race-based violence.
How do we balance our innate desire to help others with our own self-care? How do we deliver high quality care while adapting to the ever changing needs of both our patients and ourselves? How do we begin to address the impact of mass trauma events?
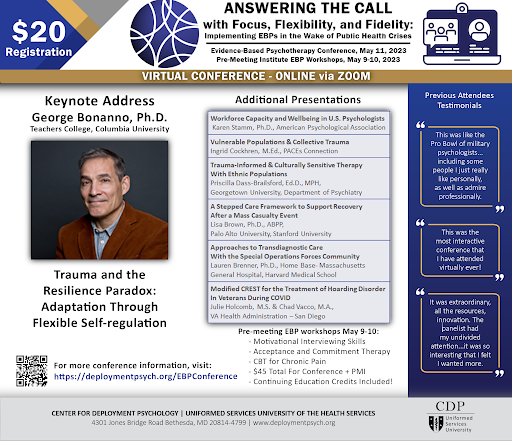
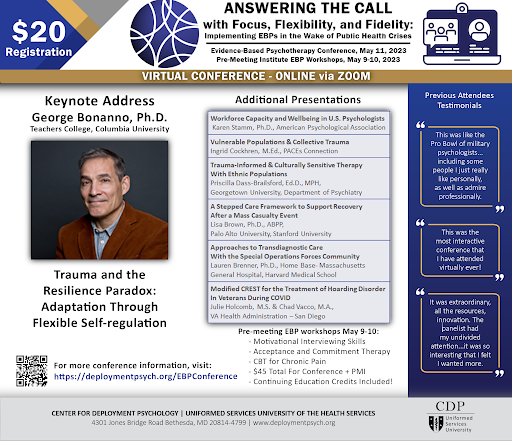
These questions influenced our planning for the Center for Deployment Psychology’s 3rd Annual Evidence-Based Psychotherapy (EBP) Conference. It is well known that we value evidence-based practices at CDP. But my colleagues and I have first-hand experience with the challenges in delivering EBPs in the context of multiple public health crises. With potentially selfish motivation, we sought to collaborate with experts who could advise us on how to deliver high-quality treatment despite the multiple obstacles we face and to answer the questions posed above.
I’m proud to share that our 2023 EBP Conference is subtitled “Answering the Call with Focus, Flexibility, and Fidelity: Implementing EBPs in the Wake of Public Health Crises.” I’m personally eager to learn more about how the PACEs framework can shape recovery in vulnerable populations, as well as get a timely update on the workforce capacity of mental health care professionals.
If you’ve been feeling similarly challenged or burned out as a clinician, you may find this year’s topics professionally relevant. Consider joining us on 11 May for this virtual conference. The low cost registration ($20) includes CE credits and several pre-meeting EBP workshops are open for registration as well. You can find out more information (and watch recordings of our past EBP Conferences) here: https://deploymentpsych.org/EBPConference
May the odds be ever in our favor while we run this ultra-marathon.
The opinions in CDP Staff Perspective blogs are solely those of the author and do not necessarily reflect the opinion of the Uniformed Services University of the Health Science or the Department of Defense.
Carin Lefkowitz, Psy.D., is a clinical psychologist and Senior Military Behavioral Health Psychologist at the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
REFERENCES:
American Psychological Association. (November 2022). Psychologists struggle to meet demand amid mental health crisis: 2022 COVID-19 provider impact survey.
https://www.apa.org/pubs/reports/practitioner/2022-covid-psychologist-workload
Practicing as a mental health clinician over the past few years has felt like running in an ultra-marathon. Not that I would ever voluntarily participate in such an endeavor. But I similarly did not voluntarily choose to confront the myriad of hurdles to clinical work since 2020: a global pandemic and its associated challenges, political and economic upheaval, heightened awareness of systemic racial violence, and continuing threats of war.
As a clinician, you’re likely well aware that the need and demand for mental health treatment has increased dramatically as a result. My practice has been full for over a year. Despite having discontinued all of my marketing, I still receive frequent inquiries, both from potential clients and other providers, because it is so difficult to locate mental health providers whose caseloads aren’t also full. Unfortunately, this isn’t unique to my geographical or specialty area. While the demand for services has increased, so has the number of mental health providers exiting the field. The American Psychological Association (APA, 2022) reported on the results of their national 2022 COVID-19 Practitioner Impact Survey. Some of the relevant lowlights include:
- 46% of psychologists reported being unable to meet the demand for treatment.
- 67% of psychologists reported having no openings for new patients.
- 38% of psychologists maintained a waitlist for their practice.
- 43% of psychologists reported seeing more patients than they did prior to the COVID-19 pandemic.
Although the APA survey focused on psychologists, it’s reasonable to assume that similar trends exist for other mental health care providers.
While our clinical practices are booming, the personal toll is significant. The APA survey noted that 45% of psychologists endorsed feeling burned out. The reality is that providers are trying their best to meet their clients’ needs while facing the same myriad of public health stressors. I know many effective CBT interventions, but that doesn’t always combat my anxiety when a family member gets diagnosed with COVID-19 or my retirement account plummets.It’s hard to keep my own mood in check when the news reports the death toll from the latest mass shooting or the most recent victim of race-based violence.
How do we balance our innate desire to help others with our own self-care? How do we deliver high quality care while adapting to the ever changing needs of both our patients and ourselves? How do we begin to address the impact of mass trauma events?
These questions influenced our planning for the Center for Deployment Psychology’s 3rd Annual Evidence-Based Psychotherapy (EBP) Conference. It is well known that we value evidence-based practices at CDP. But my colleagues and I have first-hand experience with the challenges in delivering EBPs in the context of multiple public health crises. With potentially selfish motivation, we sought to collaborate with experts who could advise us on how to deliver high-quality treatment despite the multiple obstacles we face and to answer the questions posed above.
I’m proud to share that our 2023 EBP Conference is subtitled “Answering the Call with Focus, Flexibility, and Fidelity: Implementing EBPs in the Wake of Public Health Crises.” I’m personally eager to learn more about how the PACEs framework can shape recovery in vulnerable populations, as well as get a timely update on the workforce capacity of mental health care professionals.
If you’ve been feeling similarly challenged or burned out as a clinician, you may find this year’s topics professionally relevant. Consider joining us on 11 May for this virtual conference. The low cost registration ($20) includes CE credits and several pre-meeting EBP workshops are open for registration as well. You can find out more information (and watch recordings of our past EBP Conferences) here: https://deploymentpsych.org/EBPConference
May the odds be ever in our favor while we run this ultra-marathon.
The opinions in CDP Staff Perspective blogs are solely those of the author and do not necessarily reflect the opinion of the Uniformed Services University of the Health Science or the Department of Defense.
Carin Lefkowitz, Psy.D., is a clinical psychologist and Senior Military Behavioral Health Psychologist at the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
REFERENCES:
American Psychological Association. (November 2022). Psychologists struggle to meet demand amid mental health crisis: 2022 COVID-19 provider impact survey.
https://www.apa.org/pubs/reports/practitioner/2022-covid-psychologist-workload
