Staff Perspective: Treating Post-Traumatic Nightmares
What is one of the most common symptoms that comes to mind when you think of Post-Traumatic Stress Disorder (PTSD)? If you thought of nightmares, you’re not wrong. Iin fact, up to 61% of people who have PTSD experience nightmares on a regular basis (Pigeon, Campbell, Possemato, & Ouimette, 2013). You might wonder if perhaps the worse the PTSD, the more frequent or intense the nightmares might be. Interestingly, there is indeed an association between PTSD severity and nightmares, but instead of nightmare frequency or intensity, PTSD severity correlates with the behavioral response to the nightmare: difficulty calming down and returning to sleep after a nightmare, or even anxiety about falling asleep in case the nightmare occurs (Phelps et al, 2014).
Perhaps we cannot wave a magic wand and make the nightmares go away, but as behavioral health providers we can certainly help tackle the response. Let’s give it a try…
First, let’s start with PTSD treatment. As CDP is highlighting PTSD-related resources as part of PTSD Awareness Month, you have probably by now heard about several outstanding treatment options for which CDP provides training: Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT). In the case of nightmares related to PTSD, what if we were to target the PTSD directly with PE or CPT? Absolutely, I would recommend that as a first course of action. Research on Service members with PTSD shows that while 69% had nightmares before seeking treatment, after completing the CPT protocol and no longer meeting criteria for PTSD, only 13% still had nightmares (Pruiksma et al, 2016). I should note, by the way, that for those who still had PTSD post-treatment, 52% had nightmares. This mirrors a long-term follow-up of assault survivors with PTSD who completed either PE or CPT, in that those who responded to the PTSD protocol were less likely to continue to have nightmares ten years later (Larsen et al, 2018).
This is great for treatment responders, but what about those for whom PTSD treatment is not successful? Or those who are in the minority who still do have residual nightmares after successful treatment? Or even those who have post-traumatic nightmares, but perhaps don’t meet criteria for full-blown PTSD and don’t warrant PE or CPT?
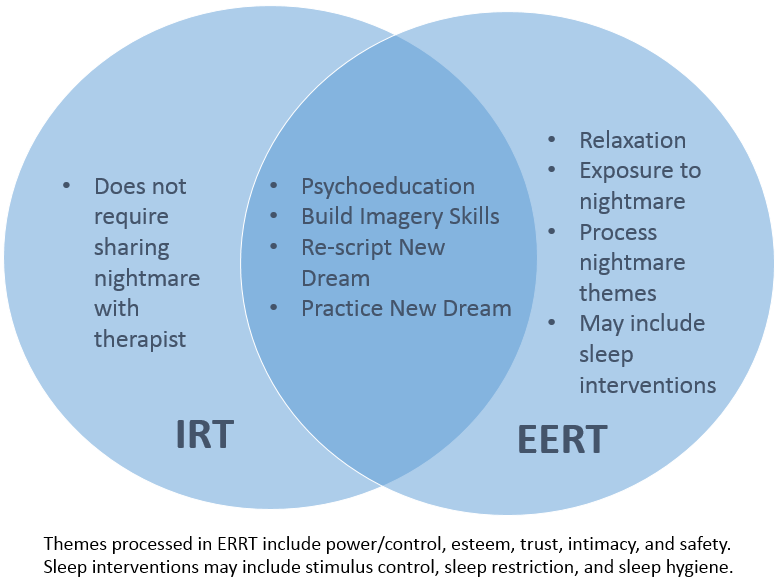
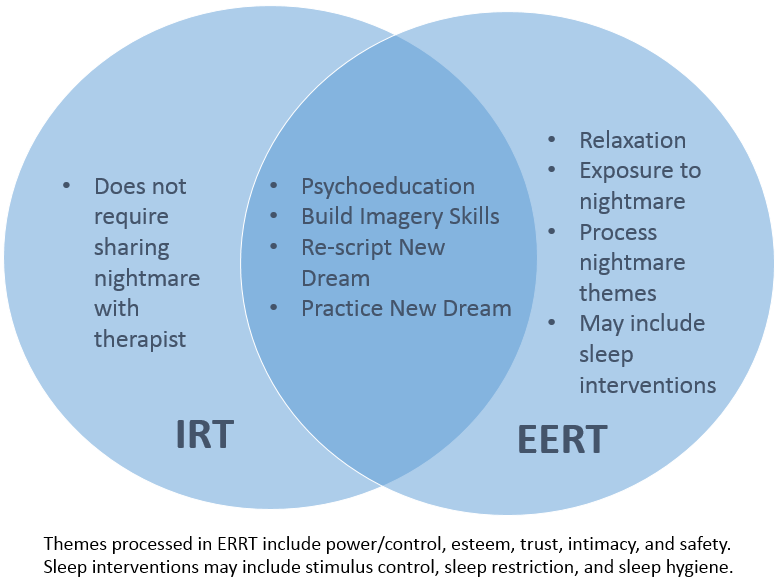
Now move to Plan B: targeting the nightmares directly. Treatment options in this category include pharmacotherapy and psychotherapy. The only recommended pharmacotherapy option, a beta-blocker called prazosin, was recently downgraded by the American Academy of Sleep Medicine and the VA/DoD guidance to “neither recommend for or against” due to a new large scale RCT finding of no differences between prazosin and a placebo for nightmares among military Veterans (Waltman et al, 2018). While further research is pending, the two recommended psychotherapy options are nightmare “rescripting” interventions: Imagery Rehearsal Therapy (IRT) and Exposure, Relaxation, and Rescripting Therapy (ERRT; Waltman et al). While IRT and ERRT have some different components, both protocols include psychoeducation, building visual imagery skills, re-scripting a new dream, and then practicing the new dream regularly (see below for a visual comparison).
Interestingly, only one of these treatments (ERRT) seems to target the responses to the nightmare mentioned above, the ability to relax or address waking fears about nightmares. Yet there is sufficient evidence for both treatments to recommend them overall. This begs the question, why do they work for some people? Some suggestions have included patients gaining a sense of mastery over nightmares, modification of nightmare-related beliefs, decreased arousal, or perhaps even indirectly via consolidation of sleep (Rousseau & Belleville, 2018). However, some have proposed that the biggest contributor to the effectiveness of rescripting treatments lies in the prevention of avoidance, which allows the activation of the fear structure, and ultimately results in emotional processing (Rousseau & Belleville).
Unfortunately, likely due to the lack of either a specified mechanism of action or guidance from a theoretical framework, the current state of the literature on behavioral nightmare approaches is disorganized at best. Studies often use similar, but different protocols precluding comparison, highly specific populations precluding generalization, and pull elements from other treatments, such as Cognitive-Behavioral Therapy for Insomnia (CBTI), making it impossible to determine which specific interventions actually work. Not surprisingly, there is no clear consensus as to which treatment might be most effective for which patients.
While dismantling studies are currently underway, there are a few resources to consider. For patients who have insomnia on top of PTSD and nightmares, there is some suggestion in the literature that improving sleep may improve nightmares, such that CBTI should be provided as a step before targeting nightmares directly (Colvonen et al, 2018). Take a look at the webinar hosted by my colleague Dr. Carin Lefkowitz and myself on treatment in co-morbid PTSD and insomnia cases. In my opinion, clinicians should consider either IRT or ERRT for residual nightmares after PTSD treatment and potentially after insomnia treatment. Even if behavioral nightmare treatment does not completely eliminate the occurrence of future nightmares, they give persons experiencing nightmares tools to manage their behavioral responses – after all, that’s what we do best.
If I’ve piqued your interest in nightmares with this blog, come join us on 19 June for my colleague Dr. Kristi Pruiksma’s webinar on PTSD-related nightmares. Dr. Pruiksma has been studying behavioral treatment of nightmares for over a decade and specifically works with Service members and military-connected populations. We hope to see you there!
The opinions in CDP Staff Perspective blogs are solely those of the author and do not necessarily reflect the opinion of the Uniformed Services University of the Health Science or the Department of Defense.
Diana Dolan, Ph.D., CBSM, is a clinical psychologist serving as a Military Behavioral Health Psychologist with the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
References
Colvonen, P.J., Straus, L.D., Stepnowsky, C., McCarthy, M.J., Goldstein, L.A., & Norman, S.B. (2018). Recent advancements in treating sleep disorders in co-occurring PTSD. Current Psychiatry Reports 20(7): 48.
Larsen, S.E., Fleming, C.J.E., & Resick, P.A. (2018). Residual symptoms following empirically supported treatment for PTSD. Psychological Trauma 11(2): 207-215.
Phelps, A.J., Creamer, M., Hopwood, M. & Forbes, D. (2014). Features of posttraumatic dreams related to PTSD severity. Journal of Traumatic Stress Disorders & Treatment 3(3)
Pruiksma, K.E., Taylor, D.J., Wachen, J.S., Mintz, J., Young-McCaughan-S., Peterson, A.L., …& Resick, P.A. (2016). Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychological Trauma 8(6): 697-701.
What is one of the most common symptoms that comes to mind when you think of Post-Traumatic Stress Disorder (PTSD)? If you thought of nightmares, you’re not wrong. Iin fact, up to 61% of people who have PTSD experience nightmares on a regular basis (Pigeon, Campbell, Possemato, & Ouimette, 2013). You might wonder if perhaps the worse the PTSD, the more frequent or intense the nightmares might be. Interestingly, there is indeed an association between PTSD severity and nightmares, but instead of nightmare frequency or intensity, PTSD severity correlates with the behavioral response to the nightmare: difficulty calming down and returning to sleep after a nightmare, or even anxiety about falling asleep in case the nightmare occurs (Phelps et al, 2014).
Perhaps we cannot wave a magic wand and make the nightmares go away, but as behavioral health providers we can certainly help tackle the response. Let’s give it a try…
First, let’s start with PTSD treatment. As CDP is highlighting PTSD-related resources as part of PTSD Awareness Month, you have probably by now heard about several outstanding treatment options for which CDP provides training: Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT). In the case of nightmares related to PTSD, what if we were to target the PTSD directly with PE or CPT? Absolutely, I would recommend that as a first course of action. Research on Service members with PTSD shows that while 69% had nightmares before seeking treatment, after completing the CPT protocol and no longer meeting criteria for PTSD, only 13% still had nightmares (Pruiksma et al, 2016). I should note, by the way, that for those who still had PTSD post-treatment, 52% had nightmares. This mirrors a long-term follow-up of assault survivors with PTSD who completed either PE or CPT, in that those who responded to the PTSD protocol were less likely to continue to have nightmares ten years later (Larsen et al, 2018).
This is great for treatment responders, but what about those for whom PTSD treatment is not successful? Or those who are in the minority who still do have residual nightmares after successful treatment? Or even those who have post-traumatic nightmares, but perhaps don’t meet criteria for full-blown PTSD and don’t warrant PE or CPT?
Now move to Plan B: targeting the nightmares directly. Treatment options in this category include pharmacotherapy and psychotherapy. The only recommended pharmacotherapy option, a beta-blocker called prazosin, was recently downgraded by the American Academy of Sleep Medicine and the VA/DoD guidance to “neither recommend for or against” due to a new large scale RCT finding of no differences between prazosin and a placebo for nightmares among military Veterans (Waltman et al, 2018). While further research is pending, the two recommended psychotherapy options are nightmare “rescripting” interventions: Imagery Rehearsal Therapy (IRT) and Exposure, Relaxation, and Rescripting Therapy (ERRT; Waltman et al). While IRT and ERRT have some different components, both protocols include psychoeducation, building visual imagery skills, re-scripting a new dream, and then practicing the new dream regularly (see below for a visual comparison).
Interestingly, only one of these treatments (ERRT) seems to target the responses to the nightmare mentioned above, the ability to relax or address waking fears about nightmares. Yet there is sufficient evidence for both treatments to recommend them overall. This begs the question, why do they work for some people? Some suggestions have included patients gaining a sense of mastery over nightmares, modification of nightmare-related beliefs, decreased arousal, or perhaps even indirectly via consolidation of sleep (Rousseau & Belleville, 2018). However, some have proposed that the biggest contributor to the effectiveness of rescripting treatments lies in the prevention of avoidance, which allows the activation of the fear structure, and ultimately results in emotional processing (Rousseau & Belleville).
Unfortunately, likely due to the lack of either a specified mechanism of action or guidance from a theoretical framework, the current state of the literature on behavioral nightmare approaches is disorganized at best. Studies often use similar, but different protocols precluding comparison, highly specific populations precluding generalization, and pull elements from other treatments, such as Cognitive-Behavioral Therapy for Insomnia (CBTI), making it impossible to determine which specific interventions actually work. Not surprisingly, there is no clear consensus as to which treatment might be most effective for which patients.
While dismantling studies are currently underway, there are a few resources to consider. For patients who have insomnia on top of PTSD and nightmares, there is some suggestion in the literature that improving sleep may improve nightmares, such that CBTI should be provided as a step before targeting nightmares directly (Colvonen et al, 2018). Take a look at the webinar hosted by my colleague Dr. Carin Lefkowitz and myself on treatment in co-morbid PTSD and insomnia cases. In my opinion, clinicians should consider either IRT or ERRT for residual nightmares after PTSD treatment and potentially after insomnia treatment. Even if behavioral nightmare treatment does not completely eliminate the occurrence of future nightmares, they give persons experiencing nightmares tools to manage their behavioral responses – after all, that’s what we do best.
If I’ve piqued your interest in nightmares with this blog, come join us on 19 June for my colleague Dr. Kristi Pruiksma’s webinar on PTSD-related nightmares. Dr. Pruiksma has been studying behavioral treatment of nightmares for over a decade and specifically works with Service members and military-connected populations. We hope to see you there!
The opinions in CDP Staff Perspective blogs are solely those of the author and do not necessarily reflect the opinion of the Uniformed Services University of the Health Science or the Department of Defense.
Diana Dolan, Ph.D., CBSM, is a clinical psychologist serving as a Military Behavioral Health Psychologist with the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
References
Colvonen, P.J., Straus, L.D., Stepnowsky, C., McCarthy, M.J., Goldstein, L.A., & Norman, S.B. (2018). Recent advancements in treating sleep disorders in co-occurring PTSD. Current Psychiatry Reports 20(7): 48.
Larsen, S.E., Fleming, C.J.E., & Resick, P.A. (2018). Residual symptoms following empirically supported treatment for PTSD. Psychological Trauma 11(2): 207-215.
Phelps, A.J., Creamer, M., Hopwood, M. & Forbes, D. (2014). Features of posttraumatic dreams related to PTSD severity. Journal of Traumatic Stress Disorders & Treatment 3(3)
Pruiksma, K.E., Taylor, D.J., Wachen, J.S., Mintz, J., Young-McCaughan-S., Peterson, A.L., …& Resick, P.A. (2016). Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychological Trauma 8(6): 697-701.

